Can a brain really be foggy? Brain fog is a common term for feeling mentally “foggy” or “cloudy.” It’s also referred to as “mental cloudiness,” “fibro fog” or “brain fuzz” and is a source of frustration for people who suffer from it.
Can histamine intolerance cause brain fog? Brain fog is that sensation where your brain is working slow and you can’t think clearly. You might feel like you’re in a daze, have problems focusing, or difficulty remembering things.
For people with histamine intolerance, brain fog is a distressing symptom, for which they desperately seek answers. No one wants to walk around most of the day, unable to think clearly, and it can be dangerous if you drive a car or work a job that requires coordination and focus.
Oftentimes, brain fog is an enigma for doctors too, as blood tests and studies often come back negative, leaving the patient and doctor scratching their heads as to what’s causing it.
If you have brain fog, always consult your doctor to make sure you don’t have another cause for your mental cloudiness. If your healthcare provider can’t find another reason your thinking is cloudy, you might wonder whether histamine intolerance can cause brain fog.
The Role of Histamine in Brain Fog
Histamine intolerance affects people in different ways. Some people with this under-diagnosed condition experience symptoms that mimic seasonal allergies, like sneezing, stuffy nose, hives, or itchy skin.
Other sufferers develop frequent digestive symptoms, like diarrhea, bloating, and flatulence. Still others have a rapid heart rate and anxiety.
Histamine intolerance manifests in a variety of ways, depending on your histamine burden and where you have the most histamine receptors.
Most tissues in your body have receptors for histamine, making it an important chemical in your body, but also one that causes problems if you have too much.
Your brain has histamine receptors too. These receptors are located in one of the larger and more important structures in the brain called the hypothalamus. (12)
In the brain, histamine receptors are responsible for controlling wakefulness, how wide awake you feel. So, it’s not a stretch to say that having too much histamine can affect brain activity and how you feel mentally.
Brain Fog is a Frustrating Symptom
It’s not unusual for people with histamine intolerance to complain of brain fog and for brain “fogginess” to interfere with their quality of life. The question is whether histamine intolerance itself is causing the brain fog, or whether another medical condition is the culprit.
It’s important to rule out other causes of brain fog before attributing it to histamine intolerance.
The term brain fog is appropriate. Patients often describe it as the sensation their brain is filled with a fog they can’t think their way out of. Thinking becomes cloudy, and it’s harder to make decisions. One patient described it as feelng removed from the rest of the world.
There are so many causes for brain fog from medical conditions to nutritional deficiencies. Lifestyle plays a role too. If you’re significantly sleep deprived or under chronic stress, you might experience brain fog until you get a good night’s sleep or resolve your stress-related issues.
Although it’s a symptom doctors hear about a lot, they don’t always have answers. Plus, most don’t consider histamine intolerance as a cause, since they don’t know a lot about the condition.

Brain Fog Has Many Causes

Some conditions associated with brain fog include:
- Vitamin B12 deficiency
- Celiac disease
- Fibromyalgia
- Chronic fatigue syndrome
- Underactive thyroid
- Blood sugar imbalance, either too high or low
- Menopause
- Multiple sclerosis
- Alzheimer’s disease
- Atherosclerotic disease (reducing blood flow to the brain)
- Depression
- Dehydration
- Certain medications
So, there are many causes of brain fog, and histamine intolerance should be a diagnosis of exclusion. You want to make sure there isn’t another reason your thinking is clouded.
Is Your Brain Fog Due to Histamine Intolerance?
If you’ve ruled out other causes of brain fog with your doctor, histamine intolerance may play a role in your symptoms. There is evidence that histamine intolerance can cause or worsen brain fog.
For example, research shows that more than 90% of people with systemic mastocytosis report moderate to severe brain fog on most days. (1) Histamine intolerance and mastocytosis have some things in common with each other.
Mastocytosis is a health condition where a person has an unusually high number of mast cells in their tissues. (2) These activated mast cells release, you guessed it, histamine.
So, people with mastocytosis have a high histamine burden, just like those with histamine intolerance, and they also experience brain fog.
Scientists speculate that histamine, whether it comes from mast cells or food, can trigger inflammation in the brain, and that inflammation, along with the inflammatory molecules it creates, can trigger brain fog.
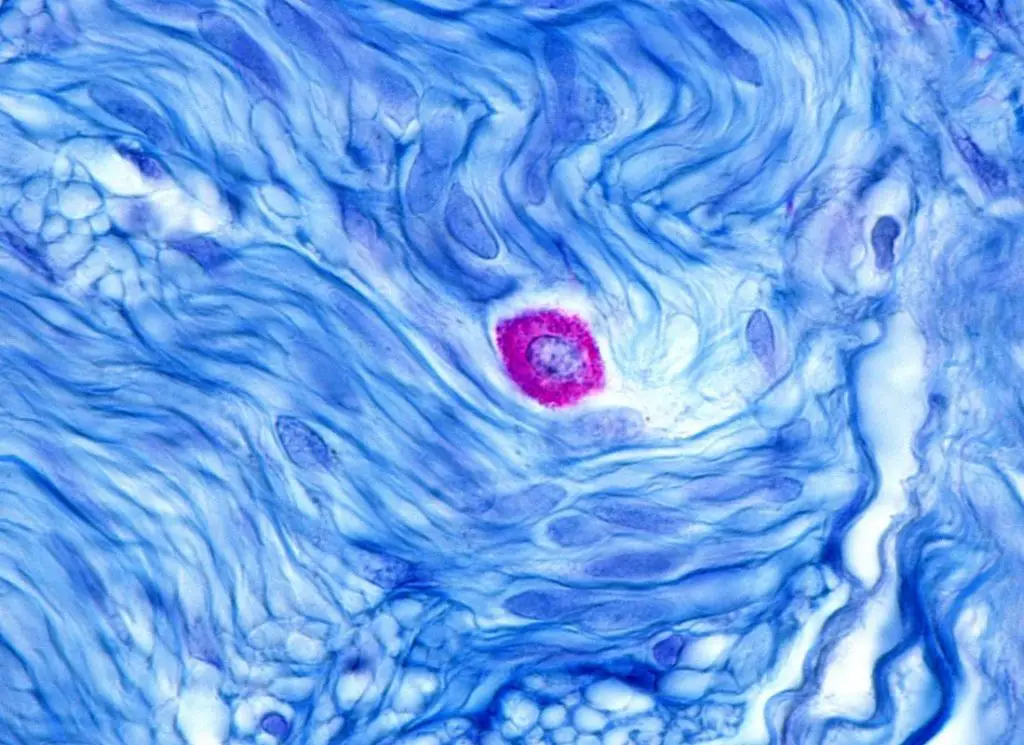
Research finds that when mast cells release histamine, it activates special immune cells in the brain called microglia that trigger brain inflammation. (5)
The Role that Histamine Plays in Brain Health
Histamine has more than one function in the human body. Along with playing a key role in the inflammatory response, studies show histamine plays a role in psychiatric and neurological conditions, including depression, anxiety, and even Alzheimer’s disease.
Although histamine helps you stay alert and learn new things, there’s a “sweet spot” for it. You need a certain amount of histamine in your nervous system for motivation, alertness, focus, and learning, but too much can overwhelm the brain and lead to brain fog.
Histamine overload can cause problems.
Too much histamine in the nervous system is linked with several neurological and psychiatric disorders and also damage or disruption of the blood-brain barrier.(9)
One way the blood-brain barrier may become damaged is by overactive mast cells releasing too much histamine and causing inflammation. One symptom of this inflammation can be brain fog.
What is the blood-brain barrier, anyway? It’s the network of blood vessels, cells, and tissues that guard against pathogens entering the brain. These pathogens include bacteria, viruses, and parasites.(6)
You want an intact blood-brain barrier to keep certain substances, including pathogens and immune cells, from reaching your brain.
Once the blood-brain barrier breaks down, inflammatory cells can enter the brain and worsen brain inflammation and the symptoms that go along with it, including brain fog.
Studies even show that histamine itself can break down the blood-brain barrier. (10)

Can a Low-Histamine Diet Reduce Brain Fog?
Scientists also point out that histamine-containing foods can increase the amount of histamine in the brain. (1) and potentially trigger symptoms of histamine excess, including brain fog.
Also, gut bacteria can make too much histamine and lead to an overabundance of histamine.
If you have enough diamine oxidase to break down the excess histamine, you would not develop symptoms. However, many people with histamine intolerance lack sufficient diamine oxidase to clear out excess histamine. (7)
If you have histamine intolerance, you may also have low levels of another enzyme called histamine N-methyltransferase that breaks down histamine inside cells.
Of the two enzymes, diamine oxidase plays a bigger role in removing excess histamine from the body. (7)
Since your level of diamine oxidase may be higher than someone else with histamine intolerance, you may tolerate more foods high in histamine than someone else with the condition.
Each case of histamine sensitivity is different, as the ability to clear histamine differs from person to person. That’s why it’s important to keep a food journal and know what triggers your symptoms.
Gut Health May Also Be a Factor
Another factor that can contribute to brain fog in people with and without histamine is dysbiosis or “bad” gut bacteria. Dysbiosis refers to unhealthy gut bacteria crowding out healthy bacteria.
What you might not know is 70% of your immune system lies in your gut. (8) When you have dysbiosis, it can activate immune cells in your gut and cause inflammation
The lining of the intestinal tract is ultra-thin. If inflammation is ongoing, it can damage the delicate lining and cause what is known as a “leaky gut.” When the lining is leaky, it allows toxins and food components to enter your bloodstream.
If you also have a break or weakening in your blood-brain barrier, those toxins can enter the brain and set up inflammation there too.
So, poor gut health can cause or aggravate inflammation in the brain. Your gut and your brain are closely connected and influence each other.

Get Back to Basics
Adopting a low-histamine diet is the first step you should take if you suspect your brain fog is due to histamine intolerance.But you also need other lifestyle changes.
Keep your diet low in histamine, but also eat more anti-inflammatory foods that reduce your body’s inflammatory burden.
Although some vegetables are off-limits if you have histamine intolerance, many are safe and beneficial because they contain antioxidants and anti-inflammatory compounds. So, enjoy more low-histamne fruits and vegetables.
Some research shows that one type of flavonoid (an anti-inflammatory compound in green vegetables) called luteolin could be beneficial for people with histamine intolerance.
A study found that a methylated analog of luteolin (6 Methoxyluteolin) blocked histamine release in response to IgE, an antibody that plays a role in allergic reactions. (11)
This is an area that needs more research but considering green vegetables have anti-inflammatory properties, eating more of them may be beneficial. Eat fresh vegetables, but stay away from fermented foods entirely.
Vegetables that are often problematic for people with histamine intolerance include spinach, tomatoes, and eggplant.
Most other green vegetables are low in histamine and don’t trigger histamine release. In fact, the myriad of antioxidants and anti-inflammatory compounds they contain are likely beneficial.

Other ways to reduce inflammation and brain fog:
- Adopt and implement techniques for managing stress. Mindfulness meditation, spending time in nature, and deep breathing exercises are approaches that work for many people.
- Take a walk outdoors in nature every day. Moderate exercise, especially in nature, has an anti-inflammatory effect and also releases natural chemicals, like endorphins, that boost clarity. Avoid high-intensity exercise, as it can worsen histamine intolerance symptoms.
- Keep a food journal, so you can correlate brain fog symptoms with what you eat.
- Go over your medications with your physician and make sure they’re not contributing to your brain fog.
- Avoid alcohol and nicotine.
- Get 7 to 8 hours of quality sleep every night. Lack of sleep increases the stress hormone cortisol, which can worsen brain fog.
Conclusion
Does histamine intolerance cause brain fog? It’s not uncommon for people with histamine intolerance to complain of brain fog. And there’s evidence that too much circulating histamine can trigger brain fog, based on the experience of people with systemic mastocytosis. But get a thorough physical and lab work to make sure there isn’t another cause for your brain fog first. Also, find out how long it takes histamine to come down after eating a high-histamine food.
References:
- Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015 Jul 3;9:225. doi: 10.3389/fnins.2015.00225. PMID: 26190965; PMCID: PMC4490655.
- NHS.UK. “Mastocytosis” https://www.nhs.uk/conditions/mastocytosis/#:~:text=Mastocytosis%20is%20a%20rare%20condition,numbers%20elsewhere%20in%20the%20body
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007 May;85(5):1185-96. doi: 10.1093/ajcn/85.5.1185. PMID: 17490952.
- Neurosci., 03 July 2015 | https://doi.org/10.3389/fnins.2015.00225
- Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Theoharis C. Theoharides1,2,3,4*, Julia M. Stewart1, Erifili Hatziagelaki5 and Gerasimos Kolaitis6.
- ASM.org. “How Pathogens Penetrate the Blood-Brain Barrier”
- The American Journal of Clinical Nutrition, Volume 85, Issue 5, May 2007, Pages 1185–1196, https://doi.org/10.1093/ajcn/85.5.1185.
- Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008 Sep;153 Suppl 1(Suppl 1):3-6. doi: 10.1111/j.1365-2249.2008.03713.x. PMID: 18721321; PMCID: PMC2515351.
- Kim SY, Buckwalter M, Soreq H, Vezzani A, Kaufer D. Blood-brain barrier dysfunction-induced inflammatory signaling in brain pathology and epileptogenesis. Epilepsia. 2012 Nov;53 Suppl 6(0 6):37-44. doi: 10.1111/j.1528-1167.2012.03701.x. PMID: 23134494; PMCID: PMC3703535. https://pubmed.ncbi.nlm.nih.gov/23134494/
- Sedeyn JC, Wu H, Hobbs RD, Levin EC, Nagele RG, Venkataraman V. Histamine Induces Alzheimer’s Disease-Like Blood Brain Barrier Breach and Local Cellular Responses in Mouse Brain Organotypic Cultures. Biomed Res Int. 2015;2015:937148. doi: 10.1155/2015/937148. Epub 2015 Nov 30. PMID: 26697497; PMCID: PMC4677161. https://pubmed.ncbi.nlm.nih.gov/26697497/
- The novel flavone tetramethoxyluteolin is a potent inhibitor of human mast cells. Weng Z, Patel AB, Panagiotidou S, Theoharides TC. J Allergy Clin Immunol. 2015 Apr; 135(4):1044-1052.e5. https://pubmed.ncbi.nlm.nih.gov/25498791/
- Panula P. Histamine receptors, agonists, and antagonists in health and disease. The Human Hypothalamus – Middle and Posterior Region. Published online 2021:377-387. doi:10.1016/b978-0-12-820107-7.00023-9

